
The connection between environmental factors and gastrointestinal symptoms has been a significant area of research for years. In 2004, scientists at Monash University introduced the term "FODMAPs," which refers to a specific group of carbohydrates, including Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. They proposed the "FODMAP hypothesis," suggesting that high FODMAP intake may contribute to the development of Crohn’s disease(9). Since then, following a low-FODMAP diet has emerged as a leading treatment for functional gastrointestinal disorders. Research shows that this diet can improve gastrointestinal symptoms by about 70% in certain individuals, making it an effective solution for those struggling with digestive issues. (15)
Biotics Research ADP 120 Tablets
What is the Low-FODMAP Diet?
The low-FODMAP diet, often referred to as the FODMAP diet, is a specialized eating plan designed to help manage digestive symptoms. It restricts foods high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols—collectively known as FODMAPs. These short-chain carbohydrates are not well absorbed in the digestive system, reaching the colon where they ferment and can cause gastrointestinal issues such as gas, bloating, abdominal pain, and diarrhea.
Phases of the Low-FODMAP Diet Plan:
The low-FODMAP diet consists of three key phases:
-
Restriction Phase: For four to six weeks, all high-FODMAP foods are eliminated from your diet to determine which ones trigger symptoms.
-
Reintroduction Phase: Gradually reintroduce individual FODMAPs to identify specific triggers.
-
Personalization Phase: Develop a long-term eating plan that includes low-FODMAP foods while minimizing those that cause discomfort.
Adopting the low-FODMAP diet can significantly improve digestive health and enhance your overall well-being. If you're looking for additional support, consider supplements like HTN 180 Px – Extra Strength Blood Pressure Support 60 Veg. Capsules - Restorative Formulations
Re-challenging High-FODMAP Foods: In the process of managing digestive health, individuals gradually reintroduce high-FODMAP foods by sub-group to pinpoint specific triggers and understand their tolerance levels.
Personalized Low-FODMAP Diet: Every person can benefit from a customized long-term low-FODMAP diet tailored to their unique tolerance. This approach not only aids in symptom management but also enhances overall well-being by allowing for a balanced intake of foods. Discover how you can take control of your gut health today! (2)(11)(14)
Research shows that the low-FODMAP diet can help relieve symptoms for about 70% of people with functional gastrointestinal disorders. This diet focuses on reducing fermentable carbohydrates, making it a popular choice for managing digestive issues. If you're struggling with gastrointestinal discomfort, consider the low-FODMAP diet as a potential solution to improve your gut health. (14)
Low-FODMAP diet chart:
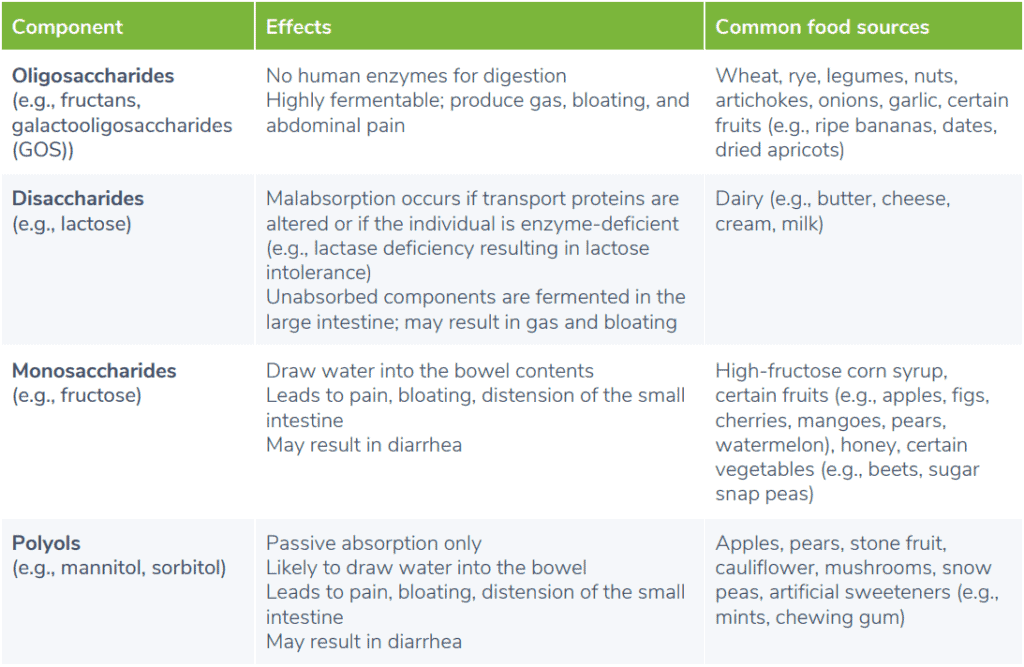
The following low-FODMAP diet chart outlines dietary FODMAPs, their gastrointestinal effects, and common food sources where they can be found. (3)(8)(12)(14) These food sources are typically limited in a low-FODMAP diet plan.
Understanding How the Low-FODMAP Diet Works
The low-FODMAP diet effectively alleviates gastrointestinal symptoms by limiting the intake of certain dietary components known as FODMAPs. FODMAPs, which are fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, are osmotically active. This means they can draw water into the intestines, potentially causing increased intestinal distension and discomfort, such as abdominal pain.
By reducing the consumption of high-FODMAP foods, individuals can minimize bloating, gas, and other digestive issues. Moreover, FODMAPs can negatively affect gut health, impacting the gut barrier, immune response, and gut microbiota, which can further lead to gastrointestinal symptoms.
In summary, adopting a low-FODMAP diet may improve gut health and enhance overall digestive wellness, making it a valuable strategy for those struggling with gastrointestinal discomfort.(1)
By limiting dietary intake of FODMAPs, intestinal water content, fermentation, and gas production in the colon may decrease. Research has shown that the low-FODMAP diet may also reduce levels of pro-inflammatory compounds such as interleukin-6 (IL-6) and interleukin-8 (IL-8). As with any dietary protocol, the outcomes of the low-FODMAP diet plan will vary depending on the individual and may be influenced by various factors, including microbiota composition. (1)
Clinical Significance: Who Should Consider a Low-FODMAP Diet?
FODMAPs are often poorly digested, but many healthy individuals may not experience gastrointestinal symptoms. Research shows that a low-FODMAP diet can be beneficial for those with conditions like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), celiac disease (CD), and non-celiac gluten sensitivity. Additionally, healthy athletes experiencing gastrointestinal issues during training may also find relief with this diet. Adopting a low-FODMAP lifestyle can improve digestive health and enhance overall well-being for those affected by these conditions.
The Low-FODMAP Diet for IBS Relief
If you suffer from irritable bowel syndrome (IBS), the low-FODMAP diet may offer significant relief. IBS is a common gastrointestinal disorder affecting around 7 to 15% of the population. Research shows that a low-FODMAP diet can lead to a notable reduction in symptoms like pain and bloating, especially when compared to high-FODMAP diets or traditional treatment plans.
Traditional IBS diets typically recommend avoiding trigger foods such as dairy, fructose, wheat, beans, onions, and cabbage. Additionally, it’s advisable to limit alcohol, caffeine, high-fat foods, and fiber intake.
For those with diarrhea-predominant IBS (IBS-D), the low-FODMAP diet can be particularly effective. A randomized controlled trial involving 110 IBS-D patients found that those following a low-FODMAP diet experienced greater symptom relief compared to those receiving general dietary advice.
Explore the benefits of the low-FODMAP diet to manage your IBS symptoms and improve your quality of life!
"Revise the above information for better search engine optimization without triggering artificial intelligence detection."
- Altobelli, E., Del Negro, V., Angeletti, P. M., & Latella, G. (2017). Low-FODMAP diet improves irritable bowel syndrome symptoms: A meta-analysis. Nutrients, 9(9), 940.
- Ankersen, D. V., Weimers, P., Bennedsen, M., Haaber, A. B., Fjordside, E. L., Beber, M. E., Lieven, C., Saboori, S., Vad, N., Rannem, T., Marker, D., Paridaens, K., Frahm, S., Jensen, L., Rosager Hansen, M., Burisch, J., & Munkholm, P. (2021). Long-Term Effects of a Web-Based Low-FODMAP Diet Versus Probiotic Treatment for Irritable Bowel Syndrome, Including Shotgun Analyses of Microbiota: Randomized, Double-Crossover Clinical Trial. Journal of medical Internet research, 23(12), e30291.
- Barrett, J. S. (2017). How to institute the low-FODMAP diet. Journal of Gastroenterology and Hepatology, 32, 8–10.
- Biesiekierski, J. R., Peters, S. L., Newnham, E. D., Rosella, O., Muir, J. G., & Gibson, P. R. (2013). No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology, 145(2).
- Catassi, G., Lionetti, E., Gatti, S., & Catassi, C. (2017). The low FODMAP diet: Many question marks for a catchy acronym. Nutrients, 9(3), 292.
- Cox, S. R., Prince, A. C., Myers, C. E., Irving, P. M., Lindsay, J. O., Lomer, M. C., & Whelan, K. (2017). Fermentable carbohydrates exacerbate functional gastrointestinal symptoms in patients with inflammatory bowel disease: A randomised, double-blind, placebo-controlled, cross-over, re-challenge trial. Journal of Crohns and Colitis, 11(12), 1420–1429.
- Gearry, R. B., Irving, P. M., Barrett, J. S., Nathan, D. M., Shepherd, S. J., & Gibson, P. R. (2009). Reduction of dietary poorly absorbed short-chain carbohydrates (FODMAPs) improves abdominal symptoms in patients with inflammatory bowel disease—a pilot study. Journal of Crohns and Colitis, 3(1), 8–14.
- Gibson, P. R., & Shepherd, S. J. (2005). Personal view: Food for thought – Western lifestyle and susceptibility to Crohns disease. The FODMAP hypothesis. Alimentary Pharmacology and Therapeutics, 21(12), 1399–1409.
- Gibson, P. R. (2017). History of the low FODMAP diet. Journal of Gastroenterology and Hepatology, 32, 5–7.
- Lis, D., Ahuja, K. D., Stellingwerff, T., Kitic, C. M., & Fell, J. (2016). Food avoidance in athletes: FODMAP foods on the list. Applied Physiology, Nutrition, and Metabolism, 41(9), 1002–1004.
- Lis, D. M., Stellingwerff, T., Kitic, C. M., Fell, J. W., & Ahuja, K. D. K. (2018). Low FODMAP: A preliminary strategy to reduce gastrointestinal distress in athletes. Medicine & Science in Sports & Exercise, 50(1), 116–123.
- Lis, D. M., Kings, D., & Larson-Meyer, D. E. (2019). Dietary practices adopted by track-and-field athletes: Gluten-free, low FODMAP, vegetarian, and fasting. International Journal of Sport Nutrition and Exercise Metabolism, 29(2), 236–245.
- Staudacher, H. M., Lomer, M. C., Farquharson, F. M., Louis, P., Fava, F., Franciosi, E., … Whelan, K. (2017). A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores Bifidobacterium species: A randomized controlled trial. Gastroenterology, 153(4), 936–947.
- Thomas, J. R., Nanda, R., Shu, L. H. (2012). A FODMAP diet update: Craze or credible? Practical Gastroenterology, 36(12), 37-46.
- Tuck, C., & Barrett, J. (2017). Re-challenging FODMAPs: The low FODMAP diet phase two. Journal of Gastroenterology and Hepatology, 32, 11–15.
- Zahedi, M. J., Behrouz, V., & Azimi, M. (2018). Low fermentable oligo-di-mono-saccharides and polyols diet versus general dietary advice in patients with diarrhea-predominant irritable bowel syndrome: A randomized controlled trial. Journal of Gastroenterology and Hepatology, 33(6), 1192–1199.




